UF researchers go nano to ease osteoarthritis
Equipped with a cutting-edge nanoparticle imaging technology, federal funds and a quest to quash pain, researchers at the University of Florida are working to revolutionize osteoarthritis treatments.
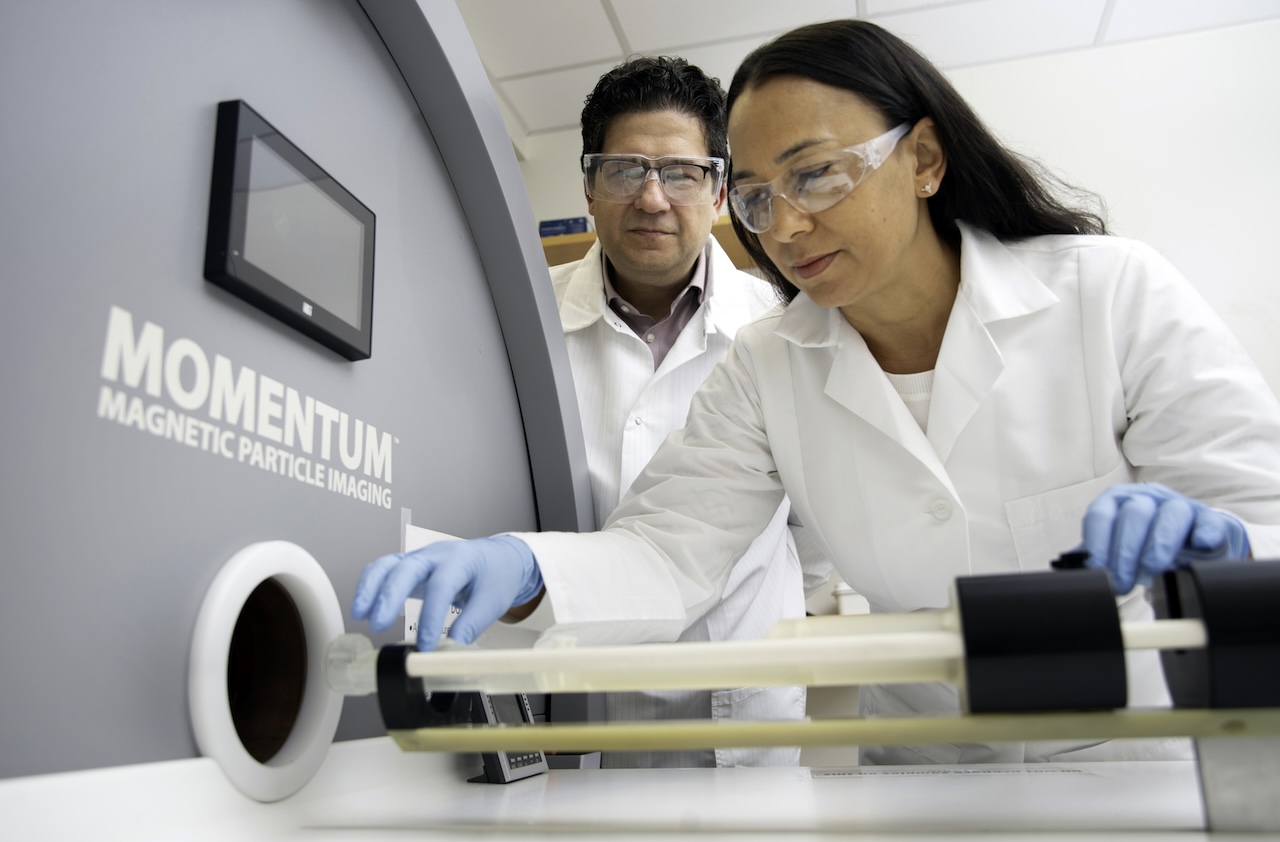
Central to the research is the Magnetic Particle Imaging (MPI) technology, a scanner with unparalleled precision in tracking nanoparticles in the body. With intravenously administered nanoparticles, the team uses the scanner to track how well the particles – with potential as diagnostic and therapeutic agents – reach inflamed joints.
“Osteoarthritis is a debilitating and degenerative joint disease with no current cure or effective long-term therapy,” said Blanka Sharma, Ph.D., an associate professor in the J. Crayton Pruitt Family Department of Biomedical Engineering and co-lead on the project. “Our research seeks to overcome the significant challenges in delivering therapeutics directly to the site of disease, which has hindered the success of many promising treatments.”
Funded by a grant from the National Institutes of Health’s Institute of Arthritis and Musculoskeletal and Skin Diseases, this research is a partnership between UF’s Biomedical and Chemical Engineering departments. Sharma’s co-principal investigator is Carlos Rinaldi-Ramos, chair of UF’s Chemical Engineering department. The team also is working with the University of Central Florida on this project.
The MPI scanner has been a transformative research tool at UF for years. It is one of five Magnetic Insight MPI scanners in North America, Rinaldi-Ramos said. And while the team is knee-deep in the osteoarthritis research, they hope the scanner will, one day, also track how well therapies and medications reach cancerous tumors.
With the osteoarthritis project, the test subjects will be mice with knee injuries. In this model, if the nanoparticle scanner can show the arrival of intravenously administered nanoparticles to the joint, then the researchers will seek to develop novel methods to monitor disease progression and deliver therapies without the need for direct injection into the joint.
“This technology helps inform the clinician on the best strategies to treat a patient,” Rinaldi-Ramos said.
Affecting more than 33 million adults in the United States, osteoarthritis is the most common type of arthritis, according to the U.S. Centers for Disease Control and Prevention. It causes joint pain, stiffness, and swelling in the hands, hips, back, or knees.
“It’s highly prevalent, and we have no therapy currently that is actually disease-modifying,” Sharma said. “Everything now is symptom management until someone needs a total joint replacement. Joint replacements are great for certain populations – the elderly and those strong enough to undergo the surgery – but it is not ideal for younger patients because of the lifespan of the implants. They also do not fully replicate the function of your joints.
“There’s a lot of interest in the field toward trying to preserve or regenerate the joint in order to delay or prevent the need for a total joint replacement. We want to retain joint function for as long as possible,” she added.
It is challenging to get therapies to the joint – what researchers refer to as bioavailability. Taking medicine orally may result in a small amount of the drug reaching the joint. Direct injections also are problematic; there are only so many times you can inject meds into the joint without tissue damage or infection.
“This grant is aimed at advancing systemic delivery of drugs,” Sharma said. And delivering those drugs intravenously to the joint may be easier on the patient.
At UCF, researchers are identifying peptide sequences that can target a mouse’s injured joint from the bloodstream. Then researchers at UF will attach those peptides to nanoparticles that serve as drug carriers and evaluate their localization to the joint from the bloodstream. The MPI scanner will quantify and measure the particles’ path.
“It’s really helping us get a better idea of where our particles are going and how long they are staying there. We think that is going to be particularly important in this application where we are delivering into the bloodstream and trying to see if they are actually localizing,” said Sharma, whose background is working with cartilage.
“This research highlights the power of innovation and collaboration in tackling complex health challenges,” said Cherie Stabler, Ph.D., chair of the J. Crayton Pruitt Family Department of Biomedical Engineering. “With technologies like the Magnetic Particle Imaging scanner, our faculty are paving the way for transformative treatments that could significantly improve patient outcomes in osteoarthritis and other diseases."
The project’s grant is for two years. But success, Sharma said, may beget another timeline.
“Moving forward,” she said, “there are opportunities to apply this either in veterinary patients, as well as larger animal models that would be needed for getting approval to go into humans.”
